Follow Your Passion: A Seamless Tumblr Journey
Medical Student - Blog Posts
REBLOG THIS. Doesn’t matter if it fits your accounts aesthetic, DO IT.
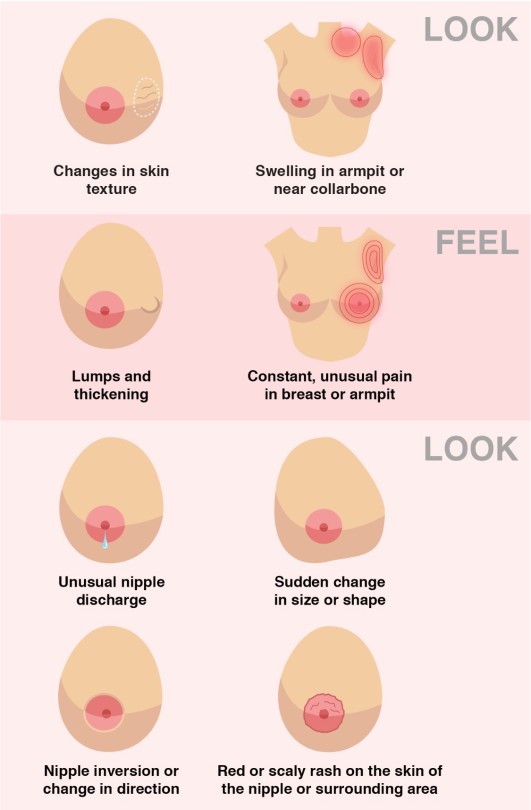
How to spot signs and symptoms of Breast Cancer
medical terminology is wild because you'll be on a chapter about the respiratory system and lungs and because of one (1) whole root word in common they'll show you a slide of some of the ugliest tooth plaque buildup ive ever seen that i had to immediately get up and floss and brush my teeth and mouthwash and i think that will forever be my mental self-image of my own teeth now. and no i don't smoke anymore and if i did i would have also stopped here too
Haemosiderin staining
"Haemosiderin staining" describes orange/red/brown skin hyperpigmentation caused by haemosiderin (an iron-containing pigment found in blood) leaking into the skin.
Causes:
Chronic venous insufficiency (in lower legs)
Skin inflammation
Trauma e.g. wound, fracture, surgery
Pigmented purpuric dermatoses
Haemochromatosis
Haemosiderin staining may be exacerbated by anticoagulant use as this increases extravasation (leakage) of red blood cells into the skin.
See an example here.
Causes of drug-induced lupus
SHIP
Sulfasalazine & Sulfonamide Hydralazine Isoniazid Procainamide & Phenytoin
This is by no means a definitive list (they are many!) but these are some of the most common causes.
Common ototoxic medications
"FAV Q&A"
Furosemide (and other loop diuretics) Aminoglycosides Vancomycin Quinine Aspirin
Hypokalaemia ECG changes
U have no pot and you have no T but you have a long PR and a long QT
Low potassium causes:
U waves (small deflection immediately after T wave)
Flattened/inverted T waves
Prolonged PR interval
Apparent prolonged QT interval (due to fusion of T and U waves)
Also:
Increased P wave amplitude
Widespread ST depression
Oedema - pitting vs non-pitting
Oedema is swelling due to excess fluids in tissues.
In pitting oedema, pressing on the affected area leaves an indentation (that persists after removing the pressure). In non-pitting oedema, the area feels firm to touch and does not form indentations.
Pitting oedema:
The excess fluid is mainly composed of water
Commonly caused by heart failure, venous insufficiency, or nephrotic syndrome
Non-pitting oedema:
The excess fluid consists of water WITH protein and salts
Usually indicates a condition of the thyroid / lymphatic system
Different types:
Lymphoedema is due to a build-up of lymphatic fluid (e.g. due to a tumour blocking lymphatic flow / after removal of lymph nodes).
Myxoedema occurs in hypothyroidism and often affected the pretibial or periorbital area.
Angioedema is localised swelling of the skin and is usually due to allergic reactions. It typically affects the face, tongue, larynx, abdomen, arms, and legs. When the larynx is affected, it may affect breathing, which is an emergency!
Lipoedema is when fat accumulates in subcutaneous tissues - it usually affects the legs/buttocks and almost exclusively occurs in postpubertal females (not the same as cellulite!)
If patients present with oedema, it's always important to test if it's pitting or non-pitting as this helps to determine the cause and correct treatment!
Causes of Acute Pancreatitis
In the UK and US, the main causes are gallstones and alcohol.
Use the mnemonic 'I GET SMASHED':
Idiopathic
Gallstones
Ethanol
Trauma
Steroids
Mumps / Malignancy
Autoimmune
Scorpion stings
Hypercalcaemia / Hypertriglyceridaemia / Hypothermia
ERCP
Drugs (including azathioprine, mesalazine, bendroflumethiazide, furosemide, steroids, sodium valproate)
Cranial nerves mnemonic
On, on, on, they travelled and found Voldemort guarding very ancient horcruxes.
Olfactory, optic, oculomotor, trochlear, trigeminal, abducens, facial, vestibulocochlear, glossopharyngeal, vagus, accessory, hypoglossal.
On - Olfactory nerve (CN I)
On - Optic nerve (CN II)
On - Oculomotor nerve (CN III)
They - Trochlear nerve (CN IV)
Travelled - Trigeminal nerve (CN V)
And - Abducens nerve (CN VI)
Found - Facial nerve (CN VII)
Voldermort - Vestibulocochlear nerve (CN VIII)
Guarding - Glossopharyngeal nerve (CN IX)
Very - Vagus nerve (CN X)
Ancient - Accessory nerve (CN XI)
Horcruxes - Hypoglossal nerve (CN XII)
clearance = (urine concentration x urine volume passed over time) / plasma concentration
the only useful thing my prof ever taught me for the renal physiology portion of my physiology course is that clearance is calculated by the equation “pissing under the sun” ( C = UV/P)
Distribution of calcium in the body
Bone calcium (99%)
Ca^2+ and PO4^3+ form hydroxyapatite
Plasma calcium
Diffusible pool
~50% of plasma calcium is free/unbound ionic Ca2+ (physiologically important form)
~10% of plasma calcium is complexed with small molecular weight compounds (citrate, phosphate)
Non-diffusible pool
~40% of plasma calcium is bound to calcium-binding proteins and plasma proteins (albumin)
The body utilises plasma albumin-bound calcium as a circulating reserve
Management of acute MI
Reduce anginal pain
Morphine (+ anti-emetic)
Oxygen
Nitrate
Initiate reperfusion
Anti-platelet (aspirin, clopidogrel)
Thrombolytic (rtPA)
Primary angioplasty (PTCA)
Anticoagulant (heparin)
Protect myocardium
Beta-blocker
ACE inhibitor
Secondary prevention
Aspirin
Lipid-lowering (statin)
Lifestyle

Helpful mnemonic foe MI treatment.


good afternoon from your resident med student. had the first phase of my research competition at 10am today. pretty simple and was very general so I’m sure I (and almost everyone else who signed up) passed. currently studying mechanisms of ventilation. will be taking a quick lunch break soon.
🪸07.06.2022🪸
Good morning!
I’ve woken up early today. I find that waking up any time before 7 always means I have a more productive day. Whilst my days haven’t been too unproductive, they haven’t been as good as they can be, hopefully today this will finally be rectified as I feel quite good. 🤭
To Do List
2018 Physics Paper 2
2019 Physics Paper 2
2018 Biology Paper 1
2019 Biology Paper 1
2020 Biology Paper 1
Later today I’m spending some time with my friends which should be really lovely. 💕
Also, I’m planning on writing some tips on how to do well in Biology, Chemistry and Physics as I feel now I’m doing quite good at them. I hope that incoming posts are useful! 💌
Have a wonderful day! 🫶🏻🤗


Picture source: Pinterest
Med student moodboard


The Physiology Of The Liver

The liver is a vital organ responsible for numerous functions including metabolism, immunity, digestion, detoxification, and vitamin storage. It weighs around 2% of an adult’s body weight and is unique due to its dual blood supply from the portal vein (75%) and the hepatic artery (25%).
Cellular Structure
The liver’s functional unit is the lobule, which is hexagonal in shape. Each corner of the hexagon has a portal triad consisting of the portal vein, hepatic artery, and bile duct. The lobule is composed mainly of hepatocytes, which have distinct apical and basolateral membranes. Hepatocytes are categorized into three zones based on their function and blood supply:
Zone I (periportal region): Closest to the blood supply, involved in oxidative metabolism (e.g., gluconeogenesis, bile formation).
Zone II (pericentral region): Sits between Zones I and III.
Zone III: Farthest from the blood supply, primarily involved in detoxification and biotransformation.
Blood and bile flow in opposite directions within the liver. The space of Disse, between the hepatocytes and the sinusoidal lumen, contains Kupffer cells (macrophages) and Ito cells (fat-storing stellate cells).
Development
The liver develops from endodermal cells of the foregut as the hepatic diverticulum around the fourth week of embryonic development. It undergoes complex differentiation influenced by various pathways (e.g., Wnt/β-catenin, FGF). By the sixth week, the liver participates in hematopoiesis, and hepatocytes begin bile production by the 12th week.
Organ Systems and Functions
The liver interacts with multiple body systems:
Digestive and Metabolic Roles: Aids in digestion, stores fat-soluble vitamins, and handles cholesterol.
Hematological Functions: Produces clotting factors and proteins.
Detoxification: Metabolizes drugs and other xenobiotics through phase I (oxidation, reduction, hydrolysis) and phase II (conjugation) reactions.
Bilirubin Metabolism: Converts heme to unconjugated bilirubin, then conjugates it for excretion.
Hormonal and Protein Synthesis: Involved in thyroid hormone activation and synthesis of nearly all plasma proteins.
Related Testing
Liver function tests (LFTs), including ALT, AST, bilirubin, alkaline phosphatase, and gamma-glutamyl transpeptidase (GGT), help assess liver health. Imaging techniques like ultrasound, CT, and MRI are also employed to identify liver abnormalities.
Pathophysiology
Cirrhosis results from chronic liver injury (e.g., due to alcoholism, hepatitis B and C), leading to fibrosis and necrosis. It causes symptoms like portal hypertension, coagulopathy, and jaundice. Hepatitis viruses (A, B, C, D, E), autoimmune diseases (e.g., primary biliary cholangitis), and metabolic conditions (e.g., non-alcoholic fatty liver disease) also contribute to liver pathology.
Clinical Significance
Understanding liver physiology helps manage conditions like viral hepatitis, alcoholic liver disease, benign liver lesions, and liver cancers. Early detection through appropriate testing and management strategies is essential for preventing end-stage liver disease and improving patient outcomes
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
Management of Preeclampsia

Preeclampsia is a hypertensive disorder of pregnancy, emerging typically after the 20th week of gestation. It is distinguished by elevated blood pressure and potential multisystem involvement, most frequently affecting renal and hepatic functions. This condition presents significant risks for maternal and fetal morbidity and mortality, necessitating keen monitoring, timely diagnosis, and appropriate management to ensure favorable outcomes for both mother and child.
Diagnostic Criteria and Processes
Clinical Criteria: The diagnosis of preeclampsia is confirmed when hypertension develops after 20 weeks of gestation in a previously normotensive woman, accompanied by one or more of the following indicators of organ dysfunction:
Proteinuria: Detection of protein in the urine, suggestive of renal impairment.
Renal Impairment: Other clinical indicators of compromised kidney function, such as increased serum creatinine.
Thrombocytopenia: A platelet count less than 100,000/microliter, indicative of platelet consumption or bone marrow suppression.
Hepatic Dysfunction: Elevated liver transaminases twice the normal concentration, reflecting hepatic injury.
Pulmonary Edema: Accumulation of fluid in the lungs, presenting as shortness of breath and hypoxemia.
Neurological Symptoms: New-onset, persistent headaches unresponsive to analgesics, or visual disturbances such as scotomata or blurred vision.
Blood Pressure Measurement: Blood pressure assessment in pregnancy involves measuring both systolic and diastolic pressures:
Systolic Pressure: A reading of 140 mm Hg or higher.
Diastolic Pressure: A reading of 90 mm Hg or higher.
For diagnostic confirmation, a second elevated reading taken at least four hours after the initial measurement is recommended.
Additional Diagnostic Tests: Upon suspicion of preeclampsia, a comprehensive evaluation is warranted, including:
Blood Tests: To assess liver enzymes, kidney function, and platelet count.
Urine Analysis: Either a 24-hour urine collection or a spot urine protein-to-creatinine ratio to evaluate protein excretion and renal function.
Fetal Ultrasound: Regular monitoring of fetal growth and amniotic fluid volume to assess intrauterine conditions.
Nonstress Test and Biophysical Profile: To evaluate fetal well-being through heart rate monitoring and ultrasound assessment of fetal movements, muscle tone, breathing, and amniotic fluid volume.
Management Strategies
Primary Management: The primary goal in managing preeclampsia is to balance prolonging the pregnancy to allow for fetal maturation with the risks posed to maternal and fetal health. This often involves a combination of close monitoring and medical interventions to control blood pressure and prevent complications.
Management of Mild Preeclampsia:
Outpatient Monitoring: Regular prenatal visits to monitor blood pressure, symptoms, and fetal health.
Home Monitoring: Daily self-monitoring of blood pressure and symptom tracking to detect any signs of disease progression.
Management of Severe Preeclampsia:
Hospitalization: For intensive monitoring of maternal and fetal well-being. This includes frequent blood pressure checks, laboratory tests, and fetal monitoring.
Pharmacotherapy:
Antihypertensive Medications: Such as labetalol, nifedipine, or methyldopa to control blood pressure.
Anticonvulsants: Magnesium sulfate is the drug of choice to prevent eclamptic seizures.
Corticosteroids: Administered to enhance fetal lung maturity if preterm delivery is anticipated.
Timing and Method of Delivery:
Delivery Timing: The timing of delivery is critical and depends on the severity of the condition, gestational age, and the health of both mother and fetus.
Mild Preeclampsia: Delivery is generally recommended after 37 weeks of gestation.
Severe Preeclampsia: May necessitate delivery before 37 weeks to prevent serious maternal and fetal complications.
2. Method of Delivery: Decided based on clinical factors, with vaginal delivery preferred if conditions allow. However, a cesarean section may be necessary for severe cases or if labor induction fails.
Postpartum Care
Monitoring and Follow-Up: Postpartum monitoring is crucial as preeclampsia can persist or even develop after delivery, known as postpartum preeclampsia. This involves:
Close Monitoring: Regular assessment of blood pressure and symptoms in the immediate postpartum period.
Patient Education: Informing patients about the signs and symptoms of postpartum preeclampsia, such as severe headaches, visual changes, epigastric pain, and nausea or vomiting, and advising them on when to seek urgent medical care.
Long-Term Follow-Up: Regular follow-up visits to monitor blood pressure and assess for potential long-term cardiovascular and renal implications of preeclampsia.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
How to Write a Case Study

The case study indulges into the ideal process of rehabilitating a semi-professional cyclist who underwent a traumatic transfemoral amputation due to a road traffic accident. This comprehensive analysis aims to shed light on the complexities of limb loss rehabilitation, emphasizing the importance of tailored interventions and evidence-based practice in optimizing outcomes for individuals facing similar challenges.
Client Characteristics

In this section, a detailed exploration of the patient’s background, lifestyle, and medical history provides crucial insights into his unique rehabilitation needs. Emphasis is placed on the impact of the accident on the patient’s physical and psychological well-being, as well as his aspirations for returning to an active lifestyle post-amputation.
The patient, a previously healthy 24-year-old male, was actively engaged in semi-professional cycling and held a physically demanding job at a bicycle shop. The road traffic accident resulted in a traumatic transfemoral amputation, significantly altering his physical capabilities and emotional state. His aspirations to return to his previous level of physical activity underscore the importance of addressing both the physical and psychological aspects of his rehabilitation journey.
Examination Findings
A thorough examination is conducted to assess the patient’s physical condition and identify areas of impairment resulting from the amputation. Objective measurements, including strength assessments and gait analysis, complement subjective reports of phantom limb pain and functional limitations, forming the basis for the subsequent formulation of a clinical hypothesis.
The examination reveals significant impairments in strength and mobility, as well as the presence of phantom limb pain, which negatively impacts the patient’s daily life and rehabilitation progress. These findings highlight the need for a comprehensive treatment approach that addresses both the physical and psychological aspects of the patient’s condition.
Clinical Hypothesis/Impression

Drawing on current research and clinical expertise, the clinical hypothesis focuses on addressing the patient’s complex pain experience and psychological distress following the amputation. The identification of neuropathic pain mechanisms and the potential efficacy of interventions such as mirror therapy and mental imagery inform the development of a tailored treatment plan aimed at promoting pain relief and enhancing functional recovery.
The clinical hypothesis highlights the importance of addressing the underlying causes of the patient’s pain and implementing evidence-based interventions to optimize his rehabilitation outcomes. By targeting both the physical and psychological aspects of his condition, the treatment plan aims to improve the patient’s overall quality of life and facilitate his successful return to daily activities.
Intervention
The intervention plan is majorly crafted to address the patient’s unique rehabilitation goals and challenges. A multi-disciplinary approach, incorporating pharmacological interventions, prosthetic care, and psychological support, is implemented to optimize outcomes and empower the patient in his journey towards recovery. Detailed descriptions of specific treatment modalities and their rationale are provided, highlighting the importance of individualized care and ongoing monitoring throughout the rehabilitation process.
The intervention plan includes a combination of pharmacological management, prosthetic fitting and training, and psychological support to address the patient’s physical and psychological needs. Each component of the plan is tailored to the patient’s specific goals and challenges, with regular monitoring and adjustments made to ensure optimal outcomes.
Outcome
Objective measures are used to track the patient’s progress and evaluate the effectiveness of the intervention plan. Significant improvements in pain management, functional mobility, and quality of life are observed over the course of treatment, with particular emphasis on the transformative impact of mirror therapy on the patient’s pain experience and overall well-being. The importance of ongoing follow-up and support is emphasized as integral to maintaining long-term gains and facilitating the patient’s successful reintegration into daily activities.
The patient demonstrates significant improvements in pain management, functional mobility, and overall quality of life following the implementation of the intervention plan. Objective measures, including pain intensity ratings and functional assessments, demonstrate tangible improvements in the patient’s physical and psychological well-being, highlighting the effectiveness of the multi-disciplinary approach employed in his rehabilitation.
Discussion
A comprehensive discussion examines the broader implications of the case study for physiotherapy practice, highlighting the importance of holistic rehabilitation approaches that address the complex interplay of physical, psychological, and social factors in individuals with limb loss. Key lessons learned from the case study, including the value of evidence-based practice and the need for ongoing collaboration between healthcare professionals, are discussed in relation to optimizing outcomes and promoting patient-centered care.
The discussion explores the broader implications of the case study for physiotherapy practice, emphasizing the importance of adopting a holistic approach to rehabilitation that addresses the complex needs of individuals with limb loss. By integrating evidence-based interventions and fostering interdisciplinary collaboration, healthcare professionals can enhance the effectiveness of rehabilitation interventions and improve outcomes for patients with limb loss.
Conclusion
In conclusion, the extended case study provides a detailed exploration of the rehabilitation journey of a semi-professional cyclist following a traumatic limb amputation. Through a comprehensive analysis of client characteristics, examination findings, intervention strategies, and outcomes, valuable insights are gained into the complexities of limb loss rehabilitation and the importance of personalized, evidence-based care in achieving optimal outcomes for individuals facing similar challenges.
The case study underscores the importance of adopting a holistic approach to rehabilitation that addresses the physical, psychological, and social aspects of limb loss by focusing on interventions to the unique needs of each patient and fostering interdisciplinary collaboration, healthcare professionals can optimize outcomes and improve the quality of life for individuals with limb loss.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
Pneumonia In Children And Adults

Introduction
Pneumonia stands as a prevalent respiratory infection, exerting a significant burden on global public health. Its impact extends beyond mere morbidity, contributing to substantial healthcare costs and socioeconomic consequences. This discussion aims to elucidate the general nature of pneumonia, encompassing its pathophysiology, clinical presentation, diagnostic modalities, treatment strategies, complications, and preventive measures. By indulging into these factors, we aim to provide a better understanding of pneumonia’s complexity and underscore the importance of timely recognition and management.
Pathophysiology

Pneumonia ensues from the infiltration of infectious agents, including bacteria, viruses, fungi, and less commonly, parasites, into the lower respiratory tract. Upon inhalation or aspiration of these pathogens, they gain access to the alveoli, where they incite an inflammatory response. This inflammatory cascade triggers the release of pro-inflammatory cytokines and chemokines, recruiting immune cells to the site of infection. Neutrophils, macrophages, and lymphocytes converge to eradicate the invading pathogens, leading to the characteristic consolidation and exudate formation within the affected lung tissue. As the infection progresses, alveolar edema, impaired gas exchange, and parenchymal damage ensue, culminating in the clinical manifestations of pneumonia.
Clinical Presentation

The clinical presentation of pneumonia encompasses a spectrum of symptoms, ranging from mild respiratory complaints to life-threatening respiratory failure. Common symptoms include cough, productive sputum production, fever, chills, pleuritic chest pain, dyspnea, tachypnea, and systemic manifestations such as malaise and fatigue. The severity of symptoms varies depending on factors such as the underlying pathogen, the extent of lung involvement, the host’s immune status, and comorbidities. In pediatric populations, pneumonia may present with nonspecific symptoms such as feeding difficulties, lethargy, and irritability, posing diagnostic challenges. Conversely, elderly individuals may exhibit atypical presentations characterized by confusion, hypothermia, and exacerbations of underlying chronic conditions.
Diagnostic Modalities

The diagnosis of pneumonia hinges on a comprehensive clinical assessment, augmented by various diagnostic modalities to confirm the presence of pulmonary infection and reveal its etiology. A thorough history and physical examination provide invaluable insights into the patient’s symptomatology, risk factors, and clinical trajectory. Symptomatic findings such as crackles, wheezes, and diminished breath sounds may aid in localizing the site of infection and assessing disease severity. Radiographic imaging, notably chest X-rays and computed tomography (CT) scans, serves as the cornerstone of pneumonia diagnosis, revealing characteristic radiographic findings such as airspace opacities, lobar consolidation, and interstitial infiltrates. Laboratory investigations, including complete blood count (CBC), C-reactive protein (CRP), and procalcitonin levels, may corroborate the clinical suspicion of pneumonia and guide therapeutic decisions. Additionally, microbiological testing of respiratory specimens through techniques such as sputum culture, blood cultures, and polymerase chain reaction (PCR) assays facilitates pathogen identification and antimicrobial susceptibility testing, thereby informing targeted therapy.
Treatment Strategies

The management of pneumonia hinges on prompt initiation of empiric antimicrobial therapy tailored to the likely causative pathogen(s) and disease severity. Antibiotics represent the mainstay of treatment for bacterial pneumonia, with the choice of agent dictated by factors such as local antimicrobial resistance patterns, patient age, comorbidities, and recent antibiotic exposure. Commonly prescribed antibiotics include beta-lactam agents (e.g., penicillins, cephalosporins), macrolides, fluoroquinolones, and combination regimens for severe or healthcare-associated infections. Conversely, viral pneumonia necessitates supportive care measures, given the limited efficacy of antiviral agents in most cases. Influenza-associated pneumonia may benefit from neuraminidase inhibitors such as oseltamivir, while respiratory syncytial virus (RSV) pneumonia may warrant ribavirin therapy in select cases. Adjunctive therapies such as oxygen supplementation, bronchodilators, and corticosteroids may mitigate respiratory distress and improve clinical outcomes, particularly in severe or hypoxemic patients. The duration of antimicrobial therapy varies depending on factors such as the causative pathogen, clinical response, radiographic resolution, and the presence of complications. Close monitoring of clinical parameters and serial imaging studies guide the decision-making process, enabling clinicians to tailor therapy to individual patient needs.
Complications

Pneumonia harbors the potential for various complications, ranging from mild to life-threatening sequelae, necessitating vigilant monitoring and timely intervention. Common complications include pleural effusion, empyema, lung abscess, respiratory failure, septic shock, and acute respiratory distress syndrome (ARDS). Pleural effusion denotes the accumulation of fluid within the pleural space, secondary to inflammation or impaired lymphatic drainage, manifesting as dyspnea, pleuritic chest pain, and dullness to percussion on physical examination. Empyema represents a purulent collection within the pleural cavity, often complicating bacterial pneumonia and necessitating drainage via thoracentesis or chest tube placement. Lung abscesses manifest as circumscribed cavities containing necrotic debris and pus within the lung parenchyma, triggered by persistent fever, productive cough, and hemoptysis. Respiratory failure ensues from impaired gas exchange and alveolar hypoventilation, caused by worsening hypoxemia, hypercapnia, and respiratory acidosis, necessitating mechanical ventilation and intensive care support. Septic shock represents a life-threatening complication of severe pneumonia, characterized by systemic inflammatory response syndrome (SIRS) and end-organ dysfunction, requiring aggressive fluid resuscitation, vasopressor therapy, and broad-spectrum antibiotics. ARDS denotes a severe form of acute lung injury, characterized by diffuse alveolar damage, refractory hypoxemia, and bilateral infiltrates on chest imaging, necessitating lung-protective ventilation and supportive care in the intensive care unit (ICU). The occurrence of complications portends a poor prognosis and underscores the need for early recognition and intervention to mitigate adverse outcomes.
Preventive Measures

Preventing pneumonia entails a broad approach encompassing vaccination, infection control measures, and health promotion strategies aimed at reducing the risk of respiratory infections and their sequelae. Vaccination stands as a cornerstone of pneumonia prevention, targeting common bacterial and viral pathogens implicated in pneumonia pathogenesis. Vaccines such as the pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) confer protection against Streptococcus pneumoniae, the leading bacterial cause of pneumonia, particularly in high-risk populations such as young children, older adults, and immunocompromised individuals. Influenza vaccination remains paramount in mitigating influenza-associated pneumonia and reducing disease transmission, underscoring the importance of annual vaccination campaigns targeting vulnerable populations. Additionally, adherence to infection control measures, including hand hygiene, respiratory etiquette, and environmental sanitation, plays a pivotal role in reducing the spread of respiratory pathogens in healthcare settings and the community at large. Health promotion efforts aimed at smoking cessation, optimizing nutrition, and addressing underlying comorbidities such as chronic obstructive pulmonary disease (COPD), asthma, and immunodeficiency bolster immune resilience and mitigate pneumonia risk. Furthermore, early identification and management of predisposing factors such as malnutrition, homelessness, and overcrowded living conditions attenuate pneumonia susceptibility and enhance overall health outcomes.
Conclusion
In conclusion, pneumonia emerges as a formidable respiratory infection, posing significant challenges to global public health. Its diverse etiology, clinical manifestations, diagnostic modalities, treatment modalities, complications, and preventive measures underscore the nature of pneumonia management. Timely recognition and intervention are imperative in mitigating the morbidity and mortality associated with pneumonia, necessitating a collaborative approach among healthcare providers, public health authorities, and policymakers. By fostering a comprehensive understanding of pneumonia’s manifest and implementing evidence-based strategies, we can strive towards reducing its burden and improving patient outcomes. Through ongoing research, education, and advocacy efforts, we can envision a future where pneumonia-related morbidity and mortality are substantially diminished, paving the way for enhanced respiratory health and well-being worldwide.
In managing pneumonia, compassion, empathy, and a holistic approach are essential alongside clinical expertise. Striving for excellence in knowledge and practice allows us to enhance respiratory medicine and patient outcomes.
As we address pneumonia and broader cardiovascular health complexities, let’s remain committed to optimal patient care. Together, we can impact lives positively and foster a healthier future.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance
Blood cell

The blood cells serves as a comprehensive guide to understanding the intricacies of hematopoiesis, the process through which various blood cell types are formed and function in the human body. This detailed discussion aims to unravel the key aspects presented in the article, delving into the structure, functions, and disorders associated with;
Red blood cells (erythrocytes),
2.White blood cells (leukocytes), and
platelets (thrombocytes).
Blood Cell Types and Composition
At the core of the circulatory system lie three major types of blood cells: red blood cells, white blood cells, and platelets. These cellular components collectively contribute to 45% of blood tissue by volume, with the remaining 55% being plasma. This delicate balance underscores the dynamic nature of blood, serving as a conduit for various vital functions within the body.
1.Red Blood Cells (Erythrocytes)
The discussion commences with a focus on red blood cells, the primary carriers of oxygen in the bloodstream. Erythrocytes, characterized by their unique biconcave shape and lack of a nucleus, play a crucial role in gas exchange facilitated by the iron-containing protein hemoglobin. The intricate details of erythropoiesis, the process of RBC formation in the red bone marrow, offer a glimpse into the remarkable physiological mechanisms that ensure a constant supply of oxygen carriers. The staggering production rate of 2.4 million RBCs per second in adults highlights the body’s continuous demand for these essential cells. The information regarding the lifespan of RBCs (100–120 days) and their subsequent removal by the spleen adds another layer to our understanding of the life cycle of these vital cells. The absence of a nucleus in mature red blood cells, a unique characteristic among human cells, is highlighted. The pathological conditions of anemia and polycythemia are thoroughly explored, shedding light on the consequences of an imbalance in red blood cell count. Additionally, the erythrocyte sedimentation rate (ESR) provides valuable insights into the diagnostic tools used in assessing the health of red blood cells.
2.White Blood Cells (Leukocytes)
The immune system, our body’s defense mechanism, relies on white blood cells to combat infectious diseases and foreign materials. These leukocytes, originating from multipotent cells in the bone marrow, are categorized into granulocytes (basophils, eosinophils, neutrophils, mast cells) and agranulocytes (lymphocytes and monocytes). The discussion delves into the roles these distinct white blood cell types play in the human immune system, offering a nuanced understanding of their functions. The conditions of leukopenia and leukocytosis, indicating low and high white blood cell counts, respectively, are explored, emphasizing the diagnostic significance of monitoring these counts. The increased white blood cell count during infections and its association with hematological cancers underscore the pivotal role leukocytes play in our overall health.
3.Platelets (Thrombocytes)
The section on platelets elucidates their role in hemostasis, the process of preventing and stopping bleeding. These small, irregularly shaped cell fragments, derived from megakaryocytes, circulate in the blood and are essential for the formation of blood clots. The average lifespan of platelets, a mere 5 to 9 days, emphasizes the continuous production required for maintaining hemostatic balance. The normal range of platelet counts and the potential consequences of low or high platelet numbers provide valuable insights into the delicate equilibrium necessary for preventing excessive bleeding or the formation of thrombosis. Thrombocytopathy, a broad term encompassing disorders related to platelets, is discussed, including thrombocytopenia, thrombasthenia, and thrombocytosis. The intricate relationship between platelets and growth factors, as well as their role in wound healing, showcases the multifaceted contributions of these small but crucial cellular fragments.
Complete Blood Count (CBC): The article introduces the Complete Blood Count (CBC) as a vital diagnostic tool providing a comprehensive analysis of blood cell composition. The historical transition from manual counting to automated analyzers reflects the evolving landscape of medical technology, enhancing the efficiency and accuracy of blood cell analysis. The significance of CBC in offering an overview of a patient’s general health status is underscored, emphasizing its widespread use in medical diagnostics.
Historical Discoveries.
The historical perspective woven into the article traces the evolution of our understanding of blood cells. From Jan Swammerdam’s pioneering observation of red blood cells in 1658 to Paul Ehrlich’s techniques in staining blood films and differential blood cell counting in 1879, the narrative highlights key milestones in the establishment of hematology as a distinct field of medicine. The contributions of various scientists, including Antoni van Leeuwenhoek, Alfred Donne, and Gabriel Andal, collectively shaped our current knowledge of blood cells.
Conclusion
The blood cells provides a rich tapestry of information encompassing their structure, functions, and associated disorders. It serves as a comprehensive resource for understanding the dynamic nature of blood and the pivotal roles played by red blood cells, white blood cells, and platelets in maintaining homeostasis within the human body. The integration of historical discoveries adds depth to the narrative, highlighting the continuous quest for knowledge that has defined the field of hematology. This article not only serves as an educational tool but also showcases the remarkable advancements in medical science and technology that have propelled our understanding of blood cells to new heights. As we unravel the mysteries of hematopoiesis, we gain valuable insights into the machinery that sustains life within our veins.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance.
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for professional assistance.
14 Reasons to become a Doctor

Introduction
Embarking on a career as a doctor is a monumental commitment, requiring an extensive education, unwavering dedication, and resilience. This detailed exploration aims to involve deep into the 14 compelling reasons to choose the noble profession of a medical doctor. Each reason represents a reality of the face and nature of the medical field, elucidating the diverse experiences, responsibilities, and its rewards associated with this esteemed profession.
1.To Help Others
At the core of a doctor’s vocation lies the fundamental responsibility to save lives and enhance the health of their patients. Exploring through challenging moments in patients’ lives, doctors have a unique opportunity to contribute significantly to their recovery and overall well-being. This shown aspect forms the very heart of the medical profession, acting as a profound motivator for those who choose this career path
2. To Explore Science

The steps involving to become a doctor unfolds as a rigorous educational stages across various scientific disciplines. From foundational studies in physics, chemistry, and biology during undergraduate education to the exploration of specialized subjects like pharmacology, anatomy, pathology, and neurology in medical school, doctors engage with an expansive array of scientific knowledge. This profession not only broadens their understanding but also empowers them to apply scientific principles practically in the life of patient care.
3 .To Have Variety in Your Work
A career in medicine is anonymously dynamic, promising a different experience each day. Doctors find themselves at the forefront of a diverse condition of illnesses and injuries, prompting the utilization of various skills and treatments. This extends beyond the medical cases to include interactions with a wide group of people, including patients, families, and colleagues, making the profession continuously admiring and intellectually engaging.
4. To Collaborate
The medical profession thrives on a team-oriented environment, fostering collaboration with nurses, orderlies, administrators, specialists, and pharmacists. This collaborative ethos not only promotes continuous learning as doctors share insights but also serves as a critical for finding collective solutions to complex medical conditions. Effective teamwork emerges as a cornerstone for successful patient care.
5.To Have Purpose in Your Work

Doctors occupy a crucial role in society, profoundly impacting the lives of individuals and their families. By promoting healthier lifestyles and improving patient health, doctors become stewards in contributing to the well-being of their communities. This sense of purpose adds a profound dimension to the daily work of a doctor.
6. To Educate
With their detailed study, doctors become experts of knowledge, which they can share with patients and colleagues as well. Patient education on health management and lifestyle improvements becomes a crucial aspect of a doctor’s responsibilities. Additionally, some doctors have the unique opportunity to contribute to medical education by mentoring and teaching medical students in teaching hospitals to get the best knowledge.
7. To Have Job Security
The universal demand for medical expertise provides doctors with a reassuring sense of job security. Unlike some professions, doctors rarely face concerns about a lack of competition for their skills. This extensive demand allows for greater flexibility when choosing a work location, catering to a broader spectrum of professional opportunities.
8. To Earn a Good Salary
While salaries in the medical field may vary based on factors such as location, experience, and specialization, doctors generally enjoy competitive remuneration coupled with excellent benefits. Specialized fields, particularly surgery, can qualify for even higher incomes. The financial rewards reflect the substantial investment of time and dedication required in pursuing of a medical career.
9. To Be a Leader

A medical career aligns seamlessly with the aspirations of individuals attached towards leadership roles. Physicians and surgeons often find themselves leading large teams of medical personnel, providing vital and main guidance while taking responsibility for patient outcomes. Exceptional leadership skills may present opportunities for doctors to pursue supervisory roles, further enriching their professional journey.
10. To Learn
Medical professionals encounter many challenges facing new medical conditions and dangers regularly. Liaising with experienced physicians and exposure to diverse cases contribute to a continuous learning environment. This commitment to lifelong learning renders a medical career particularly appealing to those with an insatiable passion for acquiring knowledge.
11. To Test Yourself
The study towards being a doctor is worth undertaking, marked by numerous challenges. Overcoming these challenges becomes a crucial for personal and professional growth. Adapting and continuous self-improvement emerge as integrated face of a physician’s journey, contributing to the development of resilient and resourceful medical professionals.
12. To Solve Problems
Critical thinking stands as a cornerstone of medical practice. Physicians accurately analyze symptoms, review patient conditions, and develop precise diagnosis, considering individual’s symptoms and clinical presentation of a disease condition. The expertise skills required in medicine demand cautiousness , structured thinking, and a balanced approach to well being , proofing the analytical competency of doctors.
13. To Contribute to Breakthroughs
Medicine, like many other scientific fields, is in a delicate state of expanding aided by technological advancements. Staying ahead of recent developments is not just a professional necessity but also an opportunity for doctors to contribute actively to breakthroughs in medical science. Those with an admiration towards medical innovation can explore positions in research hospitals, where their contributions may shape the future of healthcare.
14. To Find New Opportunities
Upon completing the rigorous phases of medical school and residency, doctors find themselves at a point of diverse opportunities. The array of choices includes pursuing specialization in a preferred field, opening a private practice, engaging in community work overseas, majoring into scientific research, contributing to public health initiatives, or transitioning into teaching positions, exploiting the versatility of a medical career.
Conclusion:
A career as a doctor is a field attached with diverse experiences, responsibilities, and opportunities. The 14 reasons explored in this discussion shed light on the main rewards and challenges that accompany the study of a medical profession. From the known satisfaction derived from helping others to the demand for knowledge and the potential to actively contribute to important developments, a medical career beckons those with indriven passion, full dedication, and a commitment to the continuous evolution of their professional journey. The resilience, adaptability, and sense of purpose implanted in the medical profession form the foundation of a vocation that extends far beyond the sense of a mere job, defining a passion that motivates those who aspire to make a meaningful impact on the lives of others through the practice of medicine.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
What Are The Stages of Fetal Growth During Pregnancy?

The development of a fetus during pregnancy is a complex and remarkable process, marked by significant changes and growth each month. This journey is typically divided into three stages known as trimesters, each lasting approximately three months. For Healthcare professionals we discuss fetal development in terms of weeks. Here’s a detailed overview of what entails during each month of pregnancy.
a) First Trimester

The first trimester of pregnancy encompasses weeks 1 through 12 and is characterized by the initial formation and rapid development of the embryo. This period is critical for establishing the foundation of the future baby’s organs and body systems. The first trimester is often associated with the onset of pregnancy symptoms, such as nausea, fatigue, and hormonal changes.
Month 1 (Weeks 1–4)
Weeks 1–2: The first two weeks of pregnancy are technically considered a preparatory period. During this time, the body releases hormones and prepares the uterus for a potential pregnancy. This period includes ovulation, where an egg is released from the ovary. If fertilization occurs, the zygote forms and marks the beginning of pregnancy.
Week 3: Fertilization occurs when a sperm cell meets the egg, creating a zygote. This single-celled entity undergoes rapid cell division as it travels down the fallopian tube towards the uterus.
Week 4: The zygote becomes a blastocyst, which is a cluster of cells that implants itself into the uterine lining. The amniotic sac and placenta begin to form, playing crucial roles in protecting and nourishing the developing embryo. By the end of this month, the blastocyst is about 2 millimeters long, roughly the size of a poppy seed.
Month 2 (Weeks 5–8)
The second month of pregnancy marks significant developmental milestones as the embryo transitions into more complex forms.
Week 5: The neural tube, which will become the brain and spinal cord, begins to form. The heart, initially a simple tube, starts to pulse, setting the stage for the development of the circulatory system.
Week 6: Limb buds appear, which will eventually become arms and legs. Structures for the ears, eyes, and mouth start to take shape. Blood cells begin to form, and circulation starts within the embryo.
Week 7: The process of ossification starts as bones begin replacing the soft cartilage, and the formation of the genitals commences. The embryo now resembles a tadpole due to its prominent tail.
Week 8: Major organs and body systems continue to develop. The hands and feet start to form web-like structures, and the umbilical cord, which provides nutrients and oxygen to the embryo, is fully developed. By the end of this month, the embryo, now referred to as a fetus, is about 0.5 to 1 inch long, similar to a black bean.
Month 3 (Weeks 9–12)
The third month of pregnancy is marked by significant growth and maturation of the embryo, transitioning into a more recognizable human form.
Week 9: Teeth and taste buds begin to form. The fetus starts developing muscles, and its body takes on a more human appearance, although the head remains disproportionately large.
Week 10: Limbs and digits are fully formed, and the external genitals start to develop, although they are not yet visible on an ultrasound. The placenta continues to grow, providing essential nutrients to the fetus.
Week 11: The fetus begins to move spontaneously, exploring its surroundings by opening and closing its fists and mouth. The bones harden, though the skin remains translucent. Facial features such as the nose and lips become more defined.
Week 12: All essential organs, limbs, bones, and muscles are present and will continue to mature and develop. The fetus is about 2.5 to 3 inches long, roughly the size of a plum. At this stage, the risk of miscarriage decreases significantly, and many women begin to feel relief from early pregnancy symptoms like morning sickness.
Second Trimester

The second trimester of pregnancy spans from weeks 13 to 26. This period is often considered the most comfortable phase of pregnancy as many early symptoms subside, and the risk of miscarriage decreases. The fetus undergoes significant growth and development, and the mother begins to feel fetal movements, known as quickening.
Month 4 (Weeks 13–16)
During the fourth month, the fetus continues to develop rapidly, and its features become more distinct.
Week 13: Vocal cords form, and the fetus’s head starts to grow proportionally to the rest of the body. The fetus begins to practice breathing movements by inhaling and exhaling amniotic fluid, which helps develop the lungs.
Week 14: The skin starts to thicken and fine hair, known as lanugo, begins to grow. The fetus can bring its fingers to its mouth and may start sucking its thumb. External genitals are fully formed, and fingerprints start to develop.
Week 15: The intestines and ears move to their final positions. The fetus practices more purposeful movements, such as thumb-sucking and smiling. The developing nervous system allows the fetus to respond to external stimuli, such as light and sound.
Week 16: The fetus can hear and respond to external sounds. Its eyes, although still closed, can perceive light. By the end of this month, the fetus is about 5 inches long and weighs around 4 ounces, comparable to an avocado.
Month 5 (Weeks 17–20)
The fifth month of pregnancy is marked by increased fetal activity and continued growth.
Week 17: Fat begins to accumulate under the skin, providing insulation and energy reserves. The fetus’s skin is covered with a protective coating called vernix, which prevents it from becoming chapped by the amniotic fluid.
Week 18: The fetus is covered in lanugo, which helps keep it warm and provides an additional layer of protection. The fetus starts to establish a sleep-wake cycle, and its movements become more noticeable to the mother.
Week 19: The fetus’s movements, including kicks and punches, become more frequent and noticeable. Unique fingerprints are fully formed, and the fetus may start to experience hiccups.
Week 20: Nails develop fully, and the sensory areas of the brain mature, allowing the fetus to respond more actively to its environment. By the end of this month, the fetus is about 9 to 10 inches long and weighs around 1 pound.
Month 6 (Weeks 21–24)
The sixth month of pregnancy is a period of significant development, particularly in the nervous and respiratory systems.
Week 21: Coordinated limb movements become more frequent, and the fetus’s bone marrow begins producing blood cells.
Week 22: The fetus’s grasping reflex strengthens, and it can touch its surroundings, including its own body and the umbilical cord. It can hear internal sounds, such as the mother’s heartbeat and external sounds, such as voices and music.
Week 23: The fetus’s viability outside the womb increases, though intensive medical care would be necessary if it were born prematurely. The fetus starts rapidly accumulating fat, which is essential for temperature regulation after birth.
Week 24: Lung development progresses, although the lungs are not yet mature enough for the fetus to breathe independently. The fetus is about 12 inches long and weighs around 2 pounds.
Third Trimester

The third trimester of pregnancy spans from weeks 27 to 40 and is characterized by rapid growth and final preparations for birth. During this period, the fetus gains weight quickly and undergoes the final stages of development necessary for survival outside the womb.
Month 7 (Weeks 25–28)
During the seventh month, the fetus continues to grow and develop reserves of body fat.
Week 25: Increased body fat makes the fetus’s skin less wrinkled and more plump. The nervous system matures rapidly, enhancing the fetus’s ability to respond to stimuli.
Week 26: Melanin production begins, contributing to the skin and eye color. The lungs start producing surfactant, a substance that helps the lungs function properly after birth.
Week 27: The fetus’s eyes open, and it develops eyelashes. The fetus begins to develop regular sleep and wake patterns, and its movements become more coordinated.
Week 28: The fetus may begin to position itself head-down in preparation for birth. By the end of this month, the fetus is about 14 to 15 inches long and weighs between 2 to 3 pounds.
Month 8 (Weeks 29–32)
The eighth month of pregnancy involves continued maturation and growth of the fetus, with a focus on brain development.
Week 29: The fetus’s movements become more distinct as space in the uterus becomes cramped. The brain develops rapidly, allowing the fetus to control its body temperature more effectively.
Week 30: The fetus’s brain continues to grow, and it can process information and respond to stimuli. The fetus begins to establish more distinct patterns of activity and rest.
Week 31: The fetus’s skin loses its translucency as fat accumulates beneath it. Most organs, except for the brain and lungs, are fully developed and ready for birth.
Week 32: The fetus is about 17 to 18 inches long and weighs up to 5 pounds. The brain continues to develop rapidly, and the fetus can hear and respond to a variety of sounds.
Month 9 (Weeks 33–36)
During the ninth month, the fetus continues to grow and mature, preparing for birth.
Week 33: The fetus’s bones harden, although the skull remains soft and flexible to facilitate passage through the birth canal.
Week 34: The protective vernix coating thickens, providing additional protection to the fetus’s skin.
Week 35: Brain growth continues, and the fetus’s brain is now capable of regulating essential body functions.
Week 36: The lanugo covering the fetus’s body begins to disappear, and hair growth occurs on the head. The fetus is about 17 to 19 inches long and weighs 6 to 7 pounds.
Month 10 (Weeks 37–40)
The final month of pregnancy is a period of final preparations for birth, with the fetus reaching full maturity.
Week 37: The fetus’s toenails reach the tips of its toes. It continues to gain weight rapidly, preparing for the energy demands of life outside the womb.
Week 38: The fetus’s weight gain continues, and it starts to shed the vernix coating. The fetus moves lower into the pelvis in preparation for birth.
Week 39: The fetus is considered full-term and continues to develop and gain weight. It measures about 18 to 20 inches long and weighs between 7 to 9 pounds.
Week 40: The fetus is ready for birth. Its organs are fully developed and capable of functioning independently. The fetus positions itself head-down in the pelvis, preparing for delivery.
Throughout pregnancy, the fetus undergoes substantial growth and development, preparing for the transition to life outside the womb. Regular monitoring and care by healthcare providers are crucial to ensure the health and well-being of both the mother and the fetus. This comprehensive journey from a single cell to a fully developed baby highlights the incredible complexity of human development.
Expert Academic Assignment Help specializes in supporting medical students to study fetal growth during pregnancy. Our assistance includes study materials, tutoring, assignment help, and exam preparation, ensuring students understand fetal development. We provide mentorship, empowering students to excel academically and become competent healthcare professionals. Email: expertassignment46@gmail.comac
14 Common Lung Diseases

Introduction
Lung diseases represent some of the most severe health threats globally. The rise of industrialization, environmental pollution, and tobacco usage significantly contribute to the prevalence of these diseases. This article, outlines the most common lung diseases, their symptoms, causes, and treatments.
1. Pneumonia

Pneumonia is an inflammation of the lung parenchyma caused by bacteria, viruses, fungi, or other pathogens. It poses a significant risk to the elderly, immunocompromised individuals, and those with chronic conditions but can also affect healthy individuals. Pneumonia can be classified based on the causative agent, such as bacterial pneumonia (e.g., Streptococcus pneumoniae), viral pneumonia (e.g., influenza virus), or fungal pneumonia (e.g., Pneumocystis jirovecii).
Symptoms
Fever
Cough with sputum
Chest pain
Shortness of breath
Fatigue
Sweating and shaking chills
Nausea, vomiting, or diarrhea (less common)
Diagnosis Diagnosis of pneumonia typically involves a combination of patient history, physical examination, chest X-rays, and sputum cultures. Blood tests may also be conducted to identify the causative agent.
Treatment Depending on the cause, treatments may include:
Antibiotics for bacterial pneumonia.
Antiviral medications for viral pneumonia.
Antifungal therapies for fungal pneumonia. Supportive care such as rest, fluids, and over-the-counter medications to reduce fever and manage pain can also alleviate symptoms. In severe cases, hospitalization may be required to provide intravenous antibiotics, oxygen therapy, or mechanical ventilation.
2. Bronchitis

Bronchitis involves the inflammation of the bronchial tubes, which carry air to and from the lungs. It can be acute, often following colds or the flu, or chronic, usually resulting from smoking or long-term exposure to irritants like pollution or dust.
Symptoms
Persistent cough (productive or dry)
Sputum production (clear, white, yellowish-gray, or green)
Fatigue
Shortness of breath
Slight fever and chills
Chest discomfort
Diagnosis Diagnosis typically involves a physical examination, where a doctor listens to the patient’s lungs with a stethoscope. Additional tests, such as a chest X-ray, sputum tests, or pulmonary function tests, may be conducted to rule out other conditions like pneumonia or asthma.
Treatment
Acute bronchitis: Symptomatic treatment includes rest, fluids, and over-the-counter pain relievers and cough medications. Inhalers or nebulizers may be prescribed to ease breathing.
Chronic bronchitis: Management may involve bronchodilators, steroids, and pulmonary rehabilitation. Smoking cessation and avoiding lung irritants are crucial for treatment.
3. Chronic Obstructive Pulmonary Disease (COPD)

COPD is a progressive, irreversible disease characterized by chronic inflammation of the airways, primarily due to smoking, environmental pollutants, or long-term exposure to respiratory irritants. COPD includes chronic bronchitis and emphysema, conditions that often coexist and lead to airflow obstruction.
Symptoms
Chronic cough
Sputum production
Shortness of breath, especially during physical activities
Wheezing
Chest tightness
Frequent respiratory infections
Fatigue
Unintended weight loss (in advanced stages)
Diagnosis COPD is diagnosed through a combination of patient history, physical examination, and spirometry, a test that measures the amount of air a person can exhale and how quickly they can do so. Chest X-rays, CT scans, and arterial blood gas analysis may also be used.
Prevention and Treatment Preventive measures include:
Smoking cessation
Vaccinations (influenza and pneumococcal vaccines)
Reducing exposure to lung irritants
Treatments involves;
Bronchodilators to relax the muscles around the airways
Inhaled steroids to reduce airway inflammation
Pulmonary rehabilitation programs
Oxygen therapy for severe cases
Surgery (e.g., lung volume reduction surgery or lung transplant) in advanced cases
4. Lung Cancer

Lung cancer involves the uncontrolled growth of malignant cells in the lung tissues. Major risk factors include smoking, exposure to secondhand smoke, exposure to carcinogens (e.g., asbestos, radon), and genetic predisposition.
Types
Small cell lung cancer (SCLC): Often linked to heavy smoking, SCLC is aggressive and spreads quickly.
Non-small cell lung cancer (NSCLC): More common and includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Symptoms
Persistent cough
Chest pain
Weight loss
Hemoptysis (coughing up blood)
Shortness of breath
Hoarseness
Bone pain (in advanced stages)
Headache (if cancer spreads to the brain)
Diagnosis Diagnosis involves imaging tests (chest X-rays, CT scans, PET scans), sputum cytology, and tissue biopsy. Molecular testing may be done to identify specific genetic mutations that can be targeted with specific treatments.
Treatment
Surgery to remove the tumor or part of the lung
Chemotherapy to kill cancer cells
Radiation therapy to destroy cancer cells or shrink tumors
Targeted drug therapies to attack specific genetic changes in cancer cells
Immunotherapy to help the immune system fight cancer
5. Pleurisy
Pleurisy, or pleuritis, is the inflammation of the pleura, the tissue lining the lungs and chest cavity. It can be caused by infections (viral, bacterial, or fungal), injuries, autoimmune diseases (e.g., lupus, rheumatoid arthritis), or other underlying conditions.
Symptoms
Sharp, stabbing chest pain that worsens with breathing, coughing, or sneezing
Shortness of breath
Cough
Fever (if infection is present)
Diagnosis Diagnosis involves a physical examination, chest X-rays, ultrasound, CT scans, and blood tests to identify the underlying cause. Thoracentesis, a procedure to remove and analyze pleural fluid, may be performed.
Treatment Treatment depends on the underlying cause and may include:
Antibiotics for bacterial infections
Antiviral medications for viral infections
Anti-inflammatory medications (e.g., NSAIDs) to reduce pain and inflammation
Pain management with medications
Thoracentesis to drain excess fluid from the pleural space
6. Pulmonary Embolism

A pulmonary embolism (PE) occurs when a blood clot, usually originating in the legs (deep vein thrombosis), travels to the lungs, blocking blood flow and causing tissue damage. Risk factors include prolonged immobility, surgery, cancer, and certain genetic conditions.
Symptoms
Sudden shortness of breath
Chest pain (may be sharp and worsen with deep breathing or coughing)
Cough (sometimes with bloody sputum)
Rapid or irregular heartbeat
Lightheadedness or dizziness
Leg pain or swelling (if DVT is present)
Diagnosis: Diagnosis involves imaging tests such as chest X-rays, CT pulmonary angiography, and ventilation-perfusion (V/Q) scans. D-dimer blood tests and ultrasound of the legs may also be conducted.
Treatment Immediate treatment includes:
Anticoagulants (blood thinners) to prevent further clotting
Thrombolytics (clot-dissolving medications) for severe cases
Surgical or catheter-based procedures to remove the clot
Long-term anticoagulation therapy to prevent recurrence
7. Pulmonary Edema

Pulmonary edema is the accumulation of fluid in the lung alveoli, making breathing difficult. It can result from heart failure (cardiogenic pulmonary edema), acute respiratory distress syndrome (ARDS), or exposure to high altitudes (non-cardiogenic pulmonary edema).
Symptoms
Difficulty breathing (dyspnea), especially when lying down
Rapid heartbeat (tachycardia)
Wheezing or gasping for breath
Coughing up frothy, pink-tinged sputum
Excessive sweating
Cyanosis (bluish skin or lips)
Diagnosis Diagnosis involves physical examination, chest X-rays, and blood tests. Echocardiography and pulmonary artery catheterization may be used to determine the underlying cause and severity.
Treatment Treatment involves addressing the underlying cause and may include:
Diuretics to remove excess fluid
Medications to improve heart function (for cardiogenic pulmonary edema)
Supplemental oxygen or mechanical ventilation
Treating underlying conditions such as infections or high altitude exposure
8. Pulmonary Fibrosis

Pulmonary fibrosis is the thickening and scarring of lung tissue, leading to reduced oxygen absorption. Causes include chronic exposure to environmental pollutants, infections, genetic factors, and autoimmune diseases (e.g., scleroderma).
Symptoms
Shortness of breath (dyspnea)
Persistent dry cough
Fatigue
Unexplained weight loss
Aching muscles and joints
Clubbing (widening and rounding) of the fingertips or toes
Diagnosis Diagnosis involves a combination of patient history, physical examination, imaging tests (chest X-rays, high-resolution CT scans), pulmonary function tests, and sometimes lung biopsy. Blood tests may be used to identify underlying autoimmune diseases.
Treatment While there is no cure for pulmonary fibrosis, treatments focus on symptom management and slowing progression:
Medications such as pirfenidone and nintedanib to slow disease progression
Oxygen therapy
Pulmonary rehabilitation
Lung transplant in severe cases
9. Pneumoconiosis
Pneumoconiosis is a lung disease caused by inhaling dust particles, such as asbestos, silica, or coal dust, leading to lung scarring. It is a type of occupational lung disease commonly seen in miners, construction workers, and industrial workers.
Symptoms:
Chronic cough
Shortness of breath
Chest tightness
Progressive loss of lung function
Diagnosis: Diagnosis involves a detailed occupational history, physical examination, chest X-rays, and CT scans. Pulmonary function tests may also be conducted to assess the extent of lung damage.
Treatment Treatment includes:
Avoiding further exposure to dust
Medications to manage symptoms, such as bronchodilators and corticosteroids
Respiratory therapies
Pulmonary rehabilitation
10. Pulmonary Arterial Hypertension (PAH)
PAH is a form of high blood pressure affecting the arteries in the lungs and the right side of the heart. It can be idiopathic, familial, or associated with other conditions such as connective tissue diseases, congenital heart disease, or chronic liver disease.
Symptoms
Breathing difficulties (dyspnea), especially during physical activities
Dizziness or fainting (syncope)
Chest pain
Fatigue
Swelling in the ankles, legs, and abdomen (edema)
Cyanosis (bluish lips and skin)
Diagnosis Diagnosis involves echocardiography, right heart catheterization, chest X-rays, and CT scans. Blood tests and pulmonary function tests may also be conducted to assess lung and heart function.
Treatment Treatment strategies include:
Medications to relax blood vessels and improve blood flow, such as endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs
Diuretics to reduce fluid retention
Oxygen therapy
Anticoagulants to prevent blood clots
In severe cases, surgical procedures such as atrial septostomy or lung transplant
11. Cystic Fibrosis
Cystic fibrosis (CF) is a genetic disorder caused by mutations in the CFTR gene, leading to thick, sticky mucus buildup in the lungs and other organs. This results in frequent infections, respiratory issues, and digestive problems.
Symptoms
Persistent cough with thick mucus
Recurrent lung infections
Wheezing or shortness of breath
Poor growth and weight gain in children
Salty-tasting skin
Severe constipation
Frequent greasy, bulky stools
Diagnosis Diagnosis involves genetic testing, sweat chloride tests, and newborn screening. Pulmonary function tests, chest X-rays, and sputum cultures may also be conducted to assess lung health.
Treatment Management includes:
Medications to thin mucus, antibiotics to treat infections, and bronchodilators to open airways
Chest physiotherapy to clear mucus
Enzyme supplements and high-calorie diets to manage digestive issues
Newer therapies targeting the underlying genetic defect, such as CFTR modulators
12. Respiratory Distress Syndrome (RDS)
RDS primarily affects premature infants due to a lack of surfactant, a substance necessary to keep the lungs open and facilitate gas exchange. Risk factors include premature birth, maternal diabetes, and multiple births.
Symptoms
Rapid, shallow breathing
Grunting sounds while breathing
Nasal flaring
Chest retractions (pulling in of the chest muscles)
Cyanosis (bluish color of the skin and mucous membranes)
Diagnosis Diagnosis involves clinical assessment, chest X-rays, and blood gas analysis to measure oxygen and carbon dioxide levels. Prenatal tests can also help identify at-risk pregnancies.
Treatment Treatment includes:
Surfactant replacement therapy to improve lung function
Mechanical ventilation or continuous positive airway pressure (CPAP) to support breathing
Oxygen therapy
Supportive care such as fluids and nutrition
13. Sarcoidosis
Sarcoidosis is characterized by the growth of granulomas (small clusters of inflammatory cells) in the lungs and other organs, likely as an immune response to unknown triggers. The exact cause remains unclear, but genetic and environmental factors are believed to play a role.
Symptoms
Dry cough
Shortness of breath
Chest pain
Fatigue
Fever
Swollen lymph nodes
Skin lesions (e.g., erythema nodosum)
Diagnosis Diagnosis involves a combination of patient history, physical examination, chest X-rays, CT scans, and pulmonary function tests. Biopsy of affected tissues may be performed to confirm the presence of granulomas.
Treatment While sarcoidosis is often self-limiting and may resolve without treatment, severe cases may require:
Corticosteroids to reduce inflammation
Immunosuppressive medications (e.g., methotrexate, azathioprine)
Antimalarial drugs (e.g., hydroxychloroquine) for skin lesions
Regular monitoring and follow-up care to manage chronic cases
14. Asthma
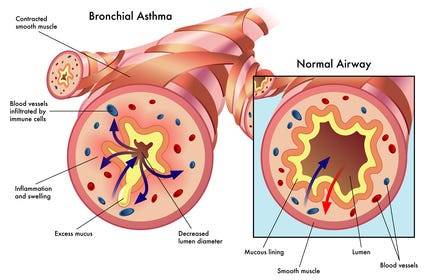
Definition and Causes: Asthma is a chronic inflammatory condition of the airways, causing episodes of wheezing, coughing, and chest tightness, often triggered by allergens, exercise, cold air, or respiratory infections. Genetic and environmental factors contribute to its development.
Symptoms
Wheezing
Shortness of breath
Chest tightness
Coughing, especially at night or early morning
Increased mucus production
Diagnosis: Diagnosis involves a detailed medical history, physical examination, and lung function tests (spirometry, peak flow measurement). Allergy testing and chest X-rays may also be conducted to identify triggers and rule out other conditions.
Treatment Management includes:
Avoiding known triggers
Inhalers (bronchodilators for quick relief, corticosteroids for long-term control)
Long-term control medications (e.g., leukotriene modifiers, long-acting beta agonists)
Immunotherapy (allergy shots) for severe allergies
Asthma action plans to manage symptoms and prevent attacks
Conclusion
Lung diseases encompass a wide range of conditions, each with distinct causes, symptoms, and treatments. Preventive measures such as avoiding smoking, reducing exposure to environmental pollutants, and timely vaccinations can significantly reduce the risk of developing many of these diseases. Early diagnosis and appropriate management are crucial in improving outcomes and quality of life for individuals affected by lung diseases. For personalized medical advice and treatment, consult with healthcare professionals.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Email us: expertassignment46@gmail.com for professional guidance.
The 12 Most Interesting Facts about Nursing

The nursing profession is a cornerstone of the healthcare system, rich in history, filled with unique facts, and bolstered by surprising statistics that highlight its evolution and impact. Whether you’re a registered nurse, nurse practitioner, nurse’s assistant, or involved in nurse staffing, there is always more to learn about this vital field. Here, we indulge into 12 intriguing facts about nursing that might surprise even those within the industry.
1. Nursing’s Ancient Origins

The earliest records of nursing date back to 300 A.D. in the Roman Empire, where nurses operated in what were considered hospitals at the time. These early healthcare institutions, known as valetudinaria, provided care primarily to soldiers and slaves. Nursing during this period was rudimentary and primarily focused on basic care and comfort.
The practice of nursing evolved significantly during the Middle Ages. Monastic orders, particularly in Europe, took on the role of caregivers. Monks and nuns provided care in hospices and infirmaries, laying the groundwork for modern nursing. The evolution continued with the establishment of more structured medical and nursing practices in response to the Black Death in the 14th century. These historical roots underscore the longstanding tradition of compassion and care in nursing.
2. Florence Nightingale’s Pioneering Influence

Florence Nightingale, often referred to as the founder of modern nursing, played a major role in transforming the profession. Born into a wealthy British family, Nightingale defied societal expectations to pursue a career in nursing. Her work during the Crimean War (1853–1856) brought her international acclaim. She was appalled by the unsanitary conditions and high mortality rates in military hospitals and implemented rigorous hygiene practices, significantly reducing the death rate.
Nightingale’s contributions extended beyond the battlefield. She established the Nightingale Training School for Nurses in 1860 at St. Thomas’ Hospital in London, emphasizing the importance of formal education and training for nurses. Her book, “Notes on Nursing: What It Is and What It Is Not,” became a seminal text in nursing education. Nightingale’s legacy includes her pioneering use of statistical analysis to advocate for healthcare reform, showcasing the impact of evidence-based practice.
3. The First Nursing School
The establishment of the Bellevue Hospital School of Nursing in New York City in 1873 marked a significant milestone in American nursing history. Inspired by Florence Nightingale’s principles, the school offered a one-year program that combined theoretical instruction with practical experience. This model set the standard for future nursing education.
Bellevue’s success prompted the establishment of other nursing schools, such as the New England Hospital for Women and Children (now part of the Boston Medical Center) and Massachusetts General Hospital’s nursing school. These institutions played a crucial role in professionalizing nursing and raising the standards of patient care. The emphasis on rigorous training and education helped transform nursing into a respected and essential profession.
4. The Physical Demands of Nursing
Nurses are known for their dedication and hard work, but the physical demands of the profession are often underestimated. On average, nurses walk four to five miles during a typical 12-hour shift, which is double the daily walking distance of most people. This constant movement is necessary to provide timely and effective care to patients, but it also highlights the physical challenges nurses face.
The demanding nature of nursing underscores the importance of proper footwear and ergonomics in the workplace. Comfortable, supportive shoes can help prevent injuries and reduce fatigue, enabling nurses to perform their duties effectively. Additionally, the physical activity associated with nursing contributes to overall health, but it also necessitates a focus on self-care and occupational health strategies to mitigate the risk of long-term musculoskeletal issues.
5. Dominance in Healthcare Education
Nursing is a dominant field within healthcare education, with approximately 50% of students in healthcare-related programs pursuing nursing degrees. This significant representation reflects the critical role nurses play in the healthcare system. The demand for nursing education has led to the development of numerous undergraduate and graduate programs, offering specialized training in various areas such as pediatric nursing, geriatric nursing, and critical care.
The strong support network among nursing students and professionals fosters a collaborative learning environment. Nursing programs emphasize not only clinical skills but also the development of critical thinking, communication, and leadership abilities. This comprehensive approach ensures that nursing graduates are well-prepared to meet the diverse and complex needs of patients.
6. Top Nursing Jobs
Nursing offers a wide range of career opportunities, and several nursing roles are consistently ranked among the top jobs in the United States. According to U.S. News & World Report, three nursing roles were among the top 40 jobs in 2021: registered nurses (ranked 37th), nurse anesthetists (ranked 39th), and nurse practitioners (ranked 3rd).
These rankings highlight the diverse and lucrative opportunities within the nursing profession. Registered nurses (RNs) are the backbone of healthcare, providing essential care and coordination in various settings. Nurse anesthetists, who administer anesthesia and monitor patients during surgical procedures, are highly specialized and command competitive salaries. Nurse practitioners (NPs) have advanced training that allows them to diagnose and treat medical conditions, often serving as primary care providers. The high ranking of NPs reflects the growing recognition of their critical role in expanding access to healthcare.
7. Mary Eliza Mahoney’s Legacy
Mary Eliza Mahoney, the first African American registered nurse in the United States, broke significant barriers in the field of nursing. Born in 1845 in Boston, Mahoney worked at the New England Hospital for Women and Children for 15 years before enrolling in its nursing program. She graduated in 1879, becoming one of only three graduates out of a class of 42.
Mahoney’s accomplishments extend beyond her personal achievements. She co-founded the National Association of Colored Graduate Nurses (NACGN) in 1908, advocating for the inclusion and recognition of African American nurses. The NACGN played a crucial role in supporting black nurses and promoting racial equality in the profession. Mahoney’s legacy is a testament to her resilience, dedication, and pioneering spirit, which continue to inspire nurses today.
8. The U.S. Nursing Workforce
As of 2020, there were approximately three million nurses in the United States, comparable to the population of Jamaica. This vast workforce is essential to the functioning of the healthcare system. Nurses work in a variety of settings, including hospitals, clinics, long-term care facilities, schools, and community health centers.
Globally, there are over 28 million nurses, accounting for 59% of healthcare professionals worldwide. This significant presence underscores the critical role nurses play in delivering healthcare services. However, the global nursing workforce faces challenges such as shortages, particularly in low- and middle-income countries. Efforts to address these shortages include increasing educational opportunities, improving working conditions, and supporting international collaboration.
9. Projected Growth in Nursing
The nursing field is not only large but also poised for continued growth. According to the U.S. Bureau of Labor Statistics, the employment of registered nurses is projected to increase by 7% from 2019 to 2029. This growth is driven by several factors, including an aging population, increased prevalence of chronic diseases, and expanded access to healthcare services.
The projected growth in nursing offers substantial opportunities for those entering the profession. It also underscores the importance of supporting nursing education and training programs to meet the demand for skilled nurses. Healthcare organizations and policymakers must invest in initiatives that attract and retain nurses, ensuring a robust workforce to provide high-quality care.
10. Diverse Work Environments
While hospitals remain the largest employer of nurses, the nursing profession offers diverse work environments. According to data from the U.S. Bureau of Labor Statistics, the distribution of nurses across various settings is as follows:
Hospitals: 60%
Ambulatory healthcare services: 18%
Nursing and residential care facilities: 7%
Government: 5%
Educational services: 3%
This diversity allows nurses to work in a range of settings, each with its unique challenges and opportunities. Ambulatory healthcare services include outpatient clinics, surgical centers, and primary care practices, where nurses play a vital role in patient care and health promotion. Nursing and residential care facilities provide long-term care for individuals with chronic illnesses or disabilities, emphasizing the importance of compassionate, ongoing support. Government and educational services offer roles in public health, policy, research, and academia, contributing to the advancement of the profession and the improvement of public health.
11. National Nurses Week
National Nurses Week, celebrated annually from May 6 to May 12, honors the challenging work and dedication of nurses. Established over 40 years ago, this week-long celebration culminates on May 12, the birthday of Florence Nightingale. The week recognizes the significant contributions of nurses to healthcare and society.
National Nurses Week includes various events and activities to celebrate and appreciate nurses. These may include educational seminars, award ceremonies, community outreach programs, and public awareness campaigns. The celebration provides an opportunity to highlight the vital role of nurses, advocate for their needs, and inspire the next generation of nursing professionals.
12. Staffing Agencies and Nursing Employment
Nurse staffing agencies play a crucial role in addressing the fluctuating demand for nursing services. Many nurses find employment through staffing agencies, which help them secure jobs and new opportunities. These agencies match nurses with healthcare facilities that need additional staff, ensuring that patient care remains uninterrupted.
For staffing agencies, keeping pace with the rising demand for nurses is crucial. Solutions like invoice factoring can provide the necessary funding to grow and support their operations effectively. Invoice factoring allows agencies to sell their accounts receivable at a discount in exchange for immediate cash, helping them manage cash flow and invest in recruiting and retaining qualified nurses.
Conclusion
These facts not only highlight the rich history and essential role of nursing but also underscore the profession’s ongoing evolution and the increasing opportunities within the field. Whether you’re a nurse or involved in nursing services, staying informed about these developments is key to advancing in this vital industry. The nursing profession continues to grow and adapt, driven by a commitment to providing high-quality care and improving patient outcomes.
For those involved in nurse staffing, understanding the dynamics of the nursing workforce and exploring financial solutions like invoice factoring can help meet the rising demand and ensure continued success. By recognizing the historical significance, current trends, and future prospects of nursing, we can better support and celebrate this indispensable profession.
For medical students and nurses of all categories, navigating assignments, homework, case studies, research, online classes, and challenging medical units can be daunting. Seeking professional guidance and assistance can make a significant difference in your academic and professional journey. For expert help with these challenges, consider reaching out to Expert Academic Assignment Help at expertassignment46@gmail.com Our professional support can help you excel in your studies and career.
The Pathophysiology Of Spondylitis

Spondylitis is a comprehensive term used to describe a group of chronic inflammatory diseases that primarily affect the joints of the spine and the sacroiliac region, which includes the pelvis and lower spine. These conditions are characterized by arthritis-like symptoms and can lead to significant discomfort, reduced mobility, and other systemic complications. This detailed exploration will indulge into the nature of spondylitis, how it differs from the related condition known as spondylosis, the various types of spondylitis, diagnostic methods, treatment options, and complementary therapies.
What is Spondylitis?

Spondylitis involves inflammation of the joints, tendons, and ligaments within the spine and sacroiliac region. Tendons are connective tissues that attach muscles to bones, while ligaments connect bones to other bones. This inflammation can result in the fusion of bones (ankylosis) and the formation of new bone, leading to stiffness and reduced flexibility in the spine. In severe cases, excessive bone growth can cause significant curvature of the spine, known as kyphosis.
Spondylitis vs. Spondylosis
While both spondylitis and spondylosis cause pain in the hip and back, they are distinct conditions with different etiologies and characteristics.
Spondylitis is an autoimmune disorder where the immune system mistakenly attacks the joints, causing inflammation, bone fusion, and excessive bone formation. This condition typically develops in teenagers and young adults and can affect multiple organs and systems within the body.
Spondylosis, on the other hand, is a degenerative condition associated with aging and the natural wear and tear of the spine. It involves the degeneration of spinal joints and discs, often accompanied by the formation of bone spurs (osteophytes). Spondylosis primarily affects older individuals, with more than 85% of people over the age of 60 experiencing this condition.
Types of Spondylitis

Medical professionals categorize spondylitis using two primary classification systems: the traditional system and the newer system. The traditional system recognizes six specific types of spondylitis, whereas the newer system categorizes spondylitis into two broad types based on the affected body region.
Traditional Spondylitis Classifications:
a) Ankylosing Spondylitis (AS)
Symptoms: Ankylosing spondylitis primarily affects the spine, causing symptoms such as fatigue, chronic back pain, stiffness, and inflammation in various areas of the body, including joints and tendons. Over time, the vertebrae may fuse, leading to reduced mobility and flexibility.
Causes: The exact cause of AS is unknown, but a strong genetic association exists with the HLA-B27 gene. Approximately 90% of individuals with AS carry this gene, although not all carriers develop the disease.
b) Reactive Arthritis
Symptoms: Reactive arthritis typically presents with a triad of symptoms including arthritis (swelling and pain in joints), conjunctivitis (inflammation of the eyes with a sticky discharge), and urethritis (genital and bladder inflammation with painful urination). However, not all patients exhibit all three symptoms.
Causes: often follows a gastrointestinal infection or a sexually transmitted infection (STI). The immune system overreacts to the initial infection, leading to inflammation and joint pain. The HLA-B27 gene is also strongly linked to ReA, with 30–50% of affected individuals carrying this gene.
c) Psoriatic Arthritis (PsA)
Symptoms: Psoriatic arthritis is associated with the inflammatory skin condition psoriasis. Symptoms include dactylitis (swelling in toes and fingers), changes in nails (such as pitting), eye pain, joint pain, reduced range of motion, and fatigue. PsA typically affects people aged 30–50.
Causes: PsA often follows psoriasis, but it can also develop in individuals without skin symptoms. There is a genetic predisposition to PsA, with at least 10% of the population inheriting genes that increase susceptibility to psoriasis and PsA.
d) Enteropathic Arthritis (EnA)
Symptoms
Enteropathic arthritis is linked to inflammatory bowel diseases (IBDs) such as ulcerative colitis and Crohn’s disease. Symptoms include abdominal pain, bloody diarrhea, and joint swelling and pain.
Causes
The precise cause of EnA is unclear, but it is associated with chronic inflammation in the bowel. This inflammation may allow bacteria to penetrate the bowel wall, triggering an immune response that leads to joint inflammation. The HLA-B27 gene is also linked to EnA.
d) Juvenile Spondyloarthritis (JSpA)
Symptoms
Juvenile spondyloarthritis begins in individuals aged 16 or younger and typically affects the leg joints. Symptoms include joint pain, tenderness, and bowel inflammation.
Causes
Similar to adult spondylitis, JSpA is often associated with the HLA-B27 gene. The exact cause remains unknown, but genetic and environmental factors likely play a role.
e)Undifferentiated Spondyloarthritis (USpA)
Symptoms
USpA is characterized by a variety of symptoms that do not fit neatly into a specific rheumatoid disorder. Symptoms may include persistent lower back pain, joint pain in small and large joints, heel pain, swelling in hands and feet, general stiffness, eye inflammation, rash, urinary tract symptoms, and intestinal inflammation.
Causes
The causes of USpA are diverse and not fully understood. It encompasses a range of symptoms that do not meet the criteria for other specific types of spondylitis.
Newer Spondylitis Categorizations
Peripheral Spondyloarthritis (pSpA)
Peripheral spondyloarthritis affects joints and tendons outside the spine and sacroiliac joints, such as the hands, wrists, elbows, shoulders, knees, ankles, and feet. It includes forms of spondylitis such as reactive arthritis, enteropathic arthritis, and undifferentiated arthritis.
2. Axial Spondyloarthritis (AxSpA)
Axial spondyloarthritis involves inflammation and pain in the pelvis and spine. This category covers a broad range of spondylitis types and includes individuals with and without sacroiliac joint fusion. AxSpA is further subdivided into non-radiographic AxSpA (without visible joint damage on X-rays) and radiographic AxSpA (visible joint damage).
Diagnosis
Diagnosing spondylitis involves abroad approach, combining physical examination, medical history, and various diagnostic tests. There is no single definitive test for spondylitis, making a comprehensive evaluation essential.
a) Physical Examination
During a physical examination, the doctor will assess the patient’s symptoms, medical history, and family history of autoimmune diseases such as psoriasis and spondyloarthritis. The examination may include evaluating joint tenderness, swelling, and range of motion.
b) Diagnostic Tests
Blood Tests: Blood tests can help identify markers of inflammation, such as elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Testing for the presence of the HLA-B27 gene can also provide valuable information, although not all individuals with spondylitis carry this gene.
Imaging Tests: Imaging techniques are crucial for diagnosing spondylitis and assessing the extent of joint and bone damage.
X-rays: X-rays can reveal changes in the spine and sacroiliac joints, such as joint fusion and bone spurs.
MRI Scans: MRI scans provide detailed images of soft tissues and can detect early signs of inflammation and joint damage that may not be visible on X-rays.
Ultrasound Scans: Ultrasound scans can be used to assess inflammation in peripheral joints and tendons.
Genetic Testing: Testing for the HLA-B27 gene can support the diagnosis, particularly in cases where clinical symptoms and imaging findings are inconclusive.
Treatment
While there is no cure for spondylitis, various treatments can help manage symptoms, reduce inflammation, and improve the patient’s quality of life. Treatment plans are often tailored to the individual’s specific symptoms and disease severity.
Medications
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs are commonly used to reduce inflammation and pain in spondylitis patients. Examples include ibuprofen and naproxen.
Corticosteroids: Corticosteroids, such as prednisone, can be prescribed for short-term use to control severe inflammation and pain.
Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs, including methotrexate and sulfasalazine, can help manage symptoms and slow disease progression in some types of spondylitis.
Biologic Agents: Biologic agents, such as tumor necrosis factor (TNF) inhibitors (e.g., adalimumab, etanercept) and interleukin-17 (IL-17) inhibitors (e.g., secukinumab), target specific components of the immune system to reduce inflammation and prevent joint damage.
Analgesics: Pain relievers, such as acetaminophen, may be used to manage pain when inflammation is not the primary issue.
Physical Therapy
Physical therapy plays a crucial role in managing spondylitis by improving and maintaining spine flexibility and overall mobility. Techniques may include:
Massage Therapy: Therapeutic massage can help reduce muscle tension, improve circulation, and alleviate pain.
Spinal Manipulation: Performed by a trained physical therapist or chiropractor, spinal manipulation can enhance mobility and reduce pain.
Exercises: Tailored exercise programs can help strengthen muscles, improve posture, and enhance flexibility. Stretching exercises are particularly beneficial for maintaining spine and joint flexibility.
Breathing Exercises: Breathing exercises are essential for individuals with ankylosing spondylitis, as the condition can affect chest expansion and respiratory function. These exercises help maintain normal lung function and prevent restrictive lung disease.
Surgery: Surgery is generally considered a last resort and is reserved for severe cases where conservative treatments have failed. Surgical options include:
Joint Replacement: For patients with severe joint damage, joint replacement surgery (e.g., hip or knee replacement) can restore function and relieve pain.
Spinal Surgery: In cases of severe spinal deformity or nerve compression, spinal surgery may be necessary to correct curvature and alleviate pressure on nerves.
Complementary Therapies
In addition to conventional treatments, complementary therapies can provide additional symptom relief and improve overall well-being. These therapies are often used alongside standard medical treatments.
Massage Therapy: Massage therapy can help reduce muscle tension, improve blood circulation, and alleviate pain and stiffness in the affected areas.
Relaxation Techniques: Techniques such as deep breathing, progressive muscle relaxation, and meditation can help manage stress and reduce pain perception.
Yoga: Yoga combines physical postures, breathing exercises, and meditation to improve flexibility, strength, and relaxation. Yoga can be particularly beneficial for maintaining spine flexibility and reducing pain.
Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body to stimulate the nervous system and promote natural pain relief and healing.
Cupping: Cupping is a traditional therapy that involves placing suction cups on the skin to improve blood flow and reduce muscle tension. It can be used to alleviate pain and stiffness in the back and other affected areas.
Summary
Spondylitis encompasses a range of chronic inflammatory diseases that affect the spine and sacroiliac region. It is characterized by autoimmune-driven inflammation, leading to joint pain, stiffness, and potential bone fusion. Spondylitis is distinct from spondylosis, a degenerative condition associated with aging. Medical professionals classify spondylitis into various types based on symptoms and affected body regions. Diagnosis involves a combination of physical examination, medical history, blood tests, imaging, and genetic testing. While there is no cure, treatments such as medications, physical therapy, and complementary therapies can help manage symptoms and improve the quality of life for those affected by spondylitis. By understanding the nature of spondylitis and the available management strategies, individuals can better navigate their condition and maintain an active, fulfilling life.
Medical students and healthcare professionals need to stay informed about the latest advancements in diagnosing and treating spondylitis. Continuous education and expert guidance are crucial for managing these complex conditions. For additional support with challenging medical units, clinical studies, research projects, assignments, and exam preparation, Expert Academic Assignment Help offers professional resources and online classes. For personalized assistance, contact expertassignment46@gmail.com Accessing expert guidance can significantly enhance your understanding and proficiency in medical education.
How Does The Brain Work?

The brain stands as a marvel of biological engineering, Composing of a multitude of bodily functions ranging from cognition and memory to emotions and sensory perception. Together with the spinal cord, it constitutes the central nervous system (CNS), the command center of the human body.
Composition of the Brain

Weighing approximately 3 pounds in adults, the brain’s main structure comprises about 60% fat, interspersed with water, protein, carbohydrates, and salts. Unlike muscles, it houses a complex network of blood vessels and nerves, including neurons and glial cells.
a) Gray and White Matter
Within the central nervous system, gray matter and white matter occupies distinct regions. In the brain, gray matter forms the outer layer, rich in neuron somas, while white matter constitutes the inner section, primarily composed of axons unsheathed in myelin. Conversely, in the spinal cord, this arrangement is reversed.
b) Brain Functionality
The brain operates by transmitting and receiving chemical and electrical signals throughout the body. These signals regulate a myriad of processes, with the brain disseminating each input. Some signals remain confined within the brain, while others traverse the spinal cord and nerves, disseminating information across the body’s expanse. This composes neural network relies on billions of interconnected neurons.
Major Brain Regions and Their Functions

1.Cerebrum
Dominating the brain’s landscape, the cerebrum encompasses the cerebral cortex and underlying white matter. It governs a spectrum of functions, including motor coordination, temperature regulation, language processing, emotional regulation, and sensory perception.
2. Brainstem
Serving as the bridge between the cerebrum and spinal cord, the brainstem comprises the midbrain, pons, and medulla. It regulates vital autonomic functions such as heart rate, breathing, and reflexive responses.
3. Cerebellum
Nestled at the posterior aspect of the brain, the cerebellum coordinates voluntary muscle movements, posture, balance, and motor learning.
Brain Coverings

a) Meninges
Three layers of protective membranes, collectively known as meninges, enshroud the brain and spinal cord. These layers — dura mater, arachnoid mater, and pia mater — shield the delicate neural tissue from physical trauma and infection.
b) Lobes of the Brain
Each hemisphere of the brain comprises four lobes, each harboring distinct functional domains:
Frontal Lobe: Governing executive functions, motor control, and higher cognitive processes.
Parietal Lobe: Integrating sensory information, spatial awareness, and perception of pain and touch.
Occipital Lobe: Specialized for visual processing and perception.
Temporal Lobe: Involved in auditory processing, language comprehension, and memory consolidation.
Deeper Brain Structures
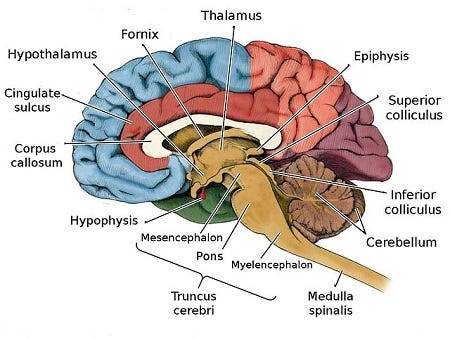
These encompass important structures such as the pituitary gland, hypothalamus, amygdala, hippocampus, and pineal gland, orchestrating hormone secretion, emotional regulation, memory consolidation, and circadian rhythms.
Blood Supply
The brain receives its oxygenated blood supply through the vertebral and carotid arteries, ensuring adequate perfusion of neural tissue. The main network of blood vessels, including the Circle of Willis, safeguards against ischemic insults and facilitates intraarterial communication.
Cranial Nerves

The twelve pairs of cranial nerves, originating from the brainstem, mediate a diverse array of sensory and motor functions, encompassing olfaction, vision, facial expression, and auditory perception.
Comprehending the anatomy and functionality of the brain fosters a deeper appreciation of its complexity and facilitates advances in neuroscientific research and therapeutic interventions aimed at diminishing neurological disorders.
Understanding the detailed anatomy and functionality of the brain is crucial for medical students embarking on their journey of study. Expert Academic Assignment Help offers invaluable assistance in navigating the complexities of neuroscience and related subjects. By leveraging expert guidance and support, students can excel in their medical education and contribute to advancements in the field of Medicine. Email us at expertassignment46@gmail.com to embark on your path to scholarly excellence and professional competency.
Gangrene

Introduction
Gangrene, a condition marked by tissue death due to insufficient blood flow or bacterial infection, poses significant risks to affected individuals. Understanding the complexities surrounding gangrene, including its symptoms, causes, diagnosis, treatment modalities, and preventive measures, is paramount for healthcare professionals and the general public alike. This comprehensive discussion aims into the aspects of gangrene, providing insights into its various dimensions and fostering awareness for timely intervention and improved patient outcomes.
Overview of Gangrene
Gangrene manifests when tissues are deprived of adequate blood supply, leading to necrosis or cell death. Whether triggered by compromised circulation or bacterial invasion, gangrene can affect diverse anatomical regions, from the extremities to internal organs. Diabetes, atherosclerosis, and other vascular disorders heighten susceptibility to gangrene, underscoring the importance of vascular health in mitigating its onset.
Symptoms of Gangrene

Recognizing the subtle yet ominous signs of gangrene is critical for timely intervention. Symptoms encompass a spectrum of manifestations, including changes in skin color, swelling, blister formation, intense pain followed by numbness, malodorous discharge, skin texture alterations, and coolness upon touch. Systemic indicators such as fever, tachycardia, and hypotension may herald severe infection or septic shock, necessitating urgent medical attention.
When to See a Doctor
Prompt medical evaluation is imperative upon the onset of persistent, unexplained pain coupled with skin discoloration, discharge, or trauma-related symptoms. Delayed intervention can exacerbate tissue damage and precipitate life-threatening complications, underscoring the urgency of seeking professional care without delay.
Causes of Gangrene

Gangrene can arise from a constellation of etiological factors, ranging from vascular insufficiency to microbial infiltration. Conditions like diabetes, atherosclerosis, traumatic injury, or surgical interventions predispose individuals to gangrene by compromising tissue perfusion or facilitating pathogen colonization. Various subtypes of gangrene, including dry, wet, gas, internal, Fournier’s, and Maloney's gangrene, exhibit distinct pathophysiological mechanisms and clinical presentations, necessitating tailored therapeutic approaches.
Diagnosis and Treatment

Accurate diagnosis of gangrene entails a special evaluation of clinical symptoms, medical history, and ancillary investigations such as imaging and laboratory tests. Treatment strategies aim to restore tissue perfusion, eradicate infection, and remove necrotic tissue. Antibiotics, hyperbaric oxygen therapy, and surgical interventions like debridement or amputation constitute cornerstone modalities, guided by the severity and anatomical extent of gangrene.
Doctors and Departments
A multidisciplinary approach involving primary care physicians, vascular surgeons, infectious disease specialists, and wound care experts is indispensable for comprehensive management of gangrene. Collaborative efforts encompass diagnostic precision, therapeutic synergy, and rehabilitative support, ensuring holistic care tailored to individual patient needs.
Prevention
Preventing gangrene necessitates proactive measures targeting predisposing factors and promoting vascular health. Effective strategies encompass glycemic control in diabetes, lifestyle modifications, smoking cessation vigorous wound care, and early recognition of ischemic or infectious triggers. Vigilant surveillance and timely intervention mitigate the risk of gangrene development, fostering tissue preservation and optimizing long-term outcomes.
Conclusion
Gangrene epitomizes a formidable clinical challenge leading to various approach consisting of prevention, early recognition, and prompt intervention. Heightened awareness of gangrene’s clinical spectrum, coupled with proactive measures targeting predisposing factors, is important for mitigating its morbidity and mortality. By fostering collaboration among healthcare providers and empowering individuals with knowledge and preventive strategies, we can confront the scourge of gangrene and safeguard tissue viability, thereby promoting optimal health and well-being for all.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance.
